|
|
||||||||||||||||
A vast amount of effort has been devoted to multiple reviews and reports. Although many of our concerns have been raised and remedies sometimes advised fundamental flaws in the system remain and recommendations have not been implemented.
Many of the problems can be traced back to the aged care act of 1997. This attempted to turn aged care into a marketplace and at the same time ensured that the sort of information which might show that this was not working was not available. The system has become opaque so that no one knows what is really happening.
The tragedy of this ill considered legislation was not only its impact on the morale and manner of operation but even more tragically the steps it took to prevent anyone from accessing the sort of information which would have shown that this was not working and that change was needed.
Politicians have had to rely on incomplete and probably flawed financial data that a reluctant industry was prepared to disclose to a 2004 investigative body that was going to tell government how much to pay them. This large and complex report was filled with impressive figures and complicated modeling by impressive academic institutions. This made it look highly credible. On that basis far reaching recommendations were made. How many of those politicians who accepted and voted on those recommendation had actually read the body of the report and how many had asked how that data was obtained. and questioned its integrity?
The community have had to rely on whistleblowers, prepared to risk their careers and that of their families for the public good, and on newspapers prepared to send their reporters into nursing homes run by two of our most credible and powerful operators. Only because a reporter went disguised as a voluntary helper to find out what was actually happening did we find out. These are the groups that a lowly accreditator, assessing the nursing home would think twice about censoring. If one of the senior staff from these groups was not on the board of the agency then his or her mates would be. Assessors would be well aware of what had happened to nurses who blew the whistle and would think hard about their own careers and what was best for their families.
Core problems then are, serious understaffing and deskilling of nursing and medical staff, a loss of morale, radically different perceptions of care in the sector, so little information about finances and standards of care that rational decisions cannot be made, broken accreditation and complaints systems, cherry picking of wealthy residents, an approved provider system that does not protect, a lack of protection from excessive commercialism, a lack of transparency and the disengagement, disenfranchisement and disempowerment of the community.
The time for change has come. Lets make sure that self interested grandstanding and obfuscation by our politicians does not derail it. They may stab each other in the back to gain power but lets make sure they don't do it to us.
The productivity commission has asked for input and every citizen has the right to do that. Those of us who are worried should write to them and tell them what we think. Go to http://www.pc.gov.au/projects/inquiry/aged-care for details. Submissions close 30th July 2010.
In looking through these many reports one is impressed on the one hand by the amount of effort that has gone into all this and on the other by the paucity of the information that has been collected and on which decisions and advice are given. Everyone has their say and uses their own data. The deficiencies lie in the collection of operating financial data and in standards of care and quality of life data.
There is no systematic independent data collected (or at least vetted) by those most affected but least represented, the residents and their communities. Everyone has their say so that there is plenty of opinion. Those who have a vested interest in an outcome that favours them dominate this. They are also those who have the knowledge and resources to make submissions.
In 1997 the newly elected coalition government removed the requirement that nursing homes be financially accountable for their subsidies and provide financial information. It was the final step in a process driven by economic rationalist thinking, mediated through think tanks and at least two reviews, the Gregory and the ALR72.
The new aged care regulations permitted, even encouraged, "providers" to siphon off money into profits - provided they could get away with the consequent impact on standards.
At the same time the measurement of standards by monitoring actual performance in terms of measurable outcomes and staffing ratios was abandoned in favour of a system of accreditation that looked at processes.
Some of the recommendations and warnings of the 1994 review by Professor Robert Gregory and the 1995 ALRC72 report were ignored.
Senate Review of Age Care Act 1997
The labor opposition had strongly opposed the bill. They held a majority in the senate so there was plenty of criticism. The senate review of this legislation warned that it would result in deskilling and understaffing, and a loss of morale in the sector. It had the "potential to compromise the standards of care". They indicated that accreditation would not prevent this and that the Gregory report had warned that it would not.
They advised against the bill but, if implemented, to counter these risks they advised a user's rights bill, an independent complaints unit, that financial accountability not be abandoned, and that advocacy groups be strengthened. These were ignored.
In retrospect it is as if the system was carefully tailored to hide the sort of information that might show that it was not working, prevent their critics from getting the information needed to show that it was not working, and effectively controlling and so muzzling criticisms. Demonstrable failure would have been acutely embarrassing for a new government imposing a new ideology on every activity across the country.
A consequence of this is that since that time we have had two polarised positions. That of the providers and government on the one hand and that of nurses, residents and families that have for one or another reason seen aspects of the aged care system that they despair of.
The providers and the government have trumpeted Australia's age care system as one of the best in the world. They bolster this with information they have collected themselves. At the same time they seek to minimise clear red flags to systemic problems by calling them unusual and isolated instances.
The nurses and families struggle to get their concerns out to the community. Their efforts are reflected in a multitude of press reports, allegations that complaints are not investigated, accusations of victimisation, and the crushing of whistleblowers. They describe the accreditation system as a farce and allege that providers game it. They do not have access to data to confirm their allegations but it takes great courage to speak out like this and few would do it lightly.
Both groups clearly have few doubts about what they see and experience. Each functions within a set of understanding which give their assertions legitimacy and there is little argument and debate between them at a grass roots, person to person, level. Each is derisive about the other so that attitudes are hardened. As this web site shows there is nothing unusual about this divide in perceptions or the way both sides behave. It is part of being human and is at least in part a consequence of the way we construct our society.
What we now have is an opaque sector dominated by a belligerent and uncompromising certainty on the one hand. This is confronted by a growing angry, emotional uncoordinated collection of outside groups appalled at what they see and experience. The situation is likely to deteriorate further unless a circuit breaker is found.
There can be no resolution until there is real sunlight shone on what is happening, and until an effective structure for regular discourse between the groups at a grassroots level is established.
Aged care has been and is still expected to be at heart a not-for-profit dominated altruistic service to the community. In practice however it is expected to operate as, be treated as, and be regulated as if it were a competitive commercial sector. Self-interested commercial entrepreneurialism is admired and encouraged.
I have argued on these web pages and in articles I have published that this introduces divisive and demoralising stresses into the sector. You cannot publicly commit to altruism while in your everyday actions you serve mammon aggressively. They are incompatible and the resulting tensions run throughout the system where they impact on morale, staffing levels and ultimately care.
This open commercialisation reverses over 2000 years of human experience and knowledge about health services. During this period structures and value systems were established to shield health, and so aged care services as they developed, from the full force of commercialism as far as was practicable.
Suffice it to assert here that it has to be accepted that, and as even Hogan almost admitted in 2004, aged care cannot operate successfully as an effective commercial profit driven enterprise.
The December 2009 Productivity Commission Research Report on public and private hospitals accepted that "competitive markets only have a limited role in the health sector". The positive review of the not-for-profit sector by the productivity commission in January 2010 gives hope that the ethos of the not-for-profit's, and the important role they play in defining how the community thinks and operates will be recognised and applied to aged care
If these early signs of a change in attitude bear fruit then we will be in a much better position to develop constructive proposals for health care and aged care. Much of what needs to be done will challenge the preconceptions of current marketplace ideology. Aged care cannot work effectively in that way.
At the same time we cannot suddenly throw out at least 30 years of thinking and 13 years of "marketplace reform" in aged care, nor should we now try to do so. We should not deny the benefits that have accrued in some sectors of society. We should examine where it has failed or had negative impacts as well as where there have been benefits.
We are currently faced by a massive blow out in need. We have no choice but to accept what has been done and move from there.
We can develop strategies, and set in place protective measures that will shine real light on the system. We can shield the system and those it serves from harm. We can try to mend the fractures in the community's trust.
Providers claim there is a funding crisis. They are once again threatening our leaders by predicting imminent collapse. The sector probably does need more funding and lots of it but this is now a ruthless competitive marketplace and that is how they have started to bargain.
We (and our representatives) need to decide what we are going to bargain for in return- a real commitment to providing real ongoing information. This is the information age - the superhighway. All "efficient" providers would have this information at their fingertips. The pre 1997 arguments no longer apply. Hand it over mates so we can all see what you are doing with our money!
The collection of financial data
The paucity of proper financial data since 1997 underlies our difficulties in planning. This was most apparent in the 2004 productivity commission review by Warren Hogan. He was given a job to do but without the information needed. No one was collecting it any more.
He had to collect information himself and was forced to go cup in hand and ask the providers whose economic future he was about to determine to supply it - only 30% did. He then had to destroy it so we could not see what they were up to and keep some of it confidential.
The likelihood that this data, from a community, vitally interested in the outcome, would be representative can be debated. We can ask about the morality of accepting it as such. This data was used as the basis for complex models and in order to make far reaching recommendations for aged care. We can speculate on the cupidity of those who unquestioningly used it as a basis for future action.
This lack of information reared its ugly head again in the Senate Standing Committee on Finance and Public Administration inquiry in April 2009. The providers and the department were in open conflict about funding and there was a slanging match about the adequacy of funding. Each produced its own set of figures to back two very different positions. There was no independent community controlled data set on which to base decisions.
The system cannot continue to operate in this way.
The Collection of data about care and quality of life
The aged care system is intended to provide "care" and a reasonable quality of life yet no attempt is made to measure either. Instead we measure a set of processes claimed to improve the standard of care and make random infrequent observations at times when most facilities are expecting us and putting on their best faces. Without measuring actual successes and failures in care we have no means of knowing whether those processes are working or not. Successive government have made no attempt to remedy this.
The only non-market information we get from inside aged care facilities comes from whistleblowers who not only risk but actually sacrifice their credibility, their careers, their financial security and the wellbeing of their families in order to expose what is happening to us in the belief that we will respond. They have then had to experience the ultimate soul destroying humiliation of seeing it become a flash in the pan as the press and the public moves on and forgets.
More recently motivated newspapers have sent their reporters into nursing homes as volunteer workers. These were homes run by some of the biggest, the most credible and the most powerful nursing home companies in Australia. Even John Howard and his succession of aged care ministers cannot claim these as exceptions or isolated instances. These were the big boys of his aged care reform process.
Look at what this reporter found by clicking here ------ and here ---- and here ---- and her diary here.
After years of complaining about profit pressures and the likely impact of private equity, even this accreditation process has been unable to hide the poor performance of at least one of these groups.
This is what aged care has come to. This is what whistle blowers sacrificed so much to expose.
Look at what happened. Is that acceptable to us?
The May 2003 independent outside audit of the new accreditation agency acknowledged that it was still struggling with a large workload. The audit drew attention to several deficiencies in the agency's operations but particularly its failure to collect the data about care, needed to measure the effectiveness of the accreditation process and to report to the community. The department agreed to do so but as far as I am aware has not risked another independent audit. The audit even at this early stage expressed concern about the conflicting roles of educator and supporter on the one hand and regulator on the other.
As the October 2007 limited review of the effectiveness of accreditation noted, no data was collected and the accreditation process in which an excess of 90% of homes got full or almost full marks lacked the sensitivity and scale required for it to be useful (but see the explanation of the 90% figure below).
They nevertheless found this method of measuring performance to be appropriate. Instead of data, the reviewers had to rely on the elicited opinions of those involved in the process to conclude that it was beneficial.
I could find no evidence that the accreditation process protects residents from dysfunctional operators, or that it is an effective method of oversight, regulation and sanctioning. This has never been evaluated. As far as I am aware there is no evidence that most residents and their families understand what the information given actually means or that it is really useful for them.
There has been another review of the accreditation system that is due to report in 2010. This has been done by the department, which is hardly an unbiased or independent entity. During 2009 the department was heavily criticised by the Senate Standing Committee on Finance and Public Administration and by Professor Walton's review of the Complaints system. It is currently in defensive mode and so may be unwilling to face the outcry from industry, and government embarrassment, should it make the recommendations needed.
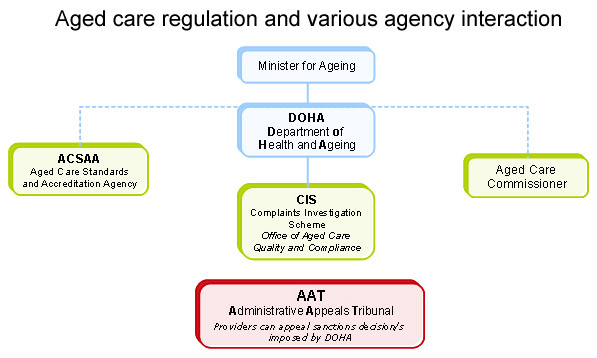
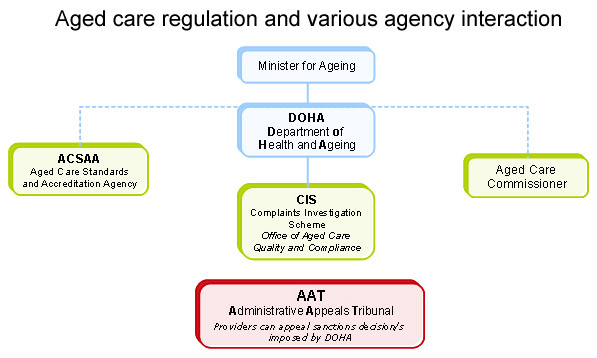
Image courtesy of Aged care Crisis Centre
The core problem for the agency is its dual and conflicting roles. Reviews have drawn attention to this. Accreditation is designed and intended to facilitate the development of good practices and as such it is closely associated with the industry. Up to half of the accreditation agency's board may be drawn from the industry at any one time which is probably reasonable for an industry support organisation.
This is not reasonable for an organisation which measures care, provides oversight, regulates, sanctions and protects the welfare of vulnerable citizens.
As long as the agency has a board on which the industry is strongly represented we cannot expect the collection of adverse information or the proper disclosure of that to the public. It cannot be considered to be credible for this purpose.
Typical of the role which the agency plays as an agent of the industry and of its operation as an advocate and marketing entity for the industry and the government is the following example.
Contrast
this with what we might expect from an impartial organisation,
monitoring,
protecting,
informing and serving the
community.
Examine the yearly reports given by
the agency and quoted to the public
by the
minister
for health (see analysis
of this by Aged Care Crisis Centre
and links there). Also
examine the reports
of the
3 year cycle
of audits prepared by the agency (see
the Special edition of
the agency's newssheet The
Standard September
2007.
Both proudly boast of low failure rates or that over 90% of all homes were compliant with all 44 standards. Those were the figures the government and the industry wanted to get out there in the public arena. Probably 99% of us would have thought that meant that less than 10% of homes had failed one or more of the accreditation standards during the period. This is not what we would have expected from the reports coming out.
Those sorts of figures were not challenged by the 2004 Hogan review nor by the accreditation review in 2007. They both swallowed it hook line and sinker (or did they?) yet this is one of the oldest tricks of the trade and is used to challenge first year students in logic courses.
Think again and read the words not the meaning. Most of us read meaning not individual words. It was only when someone else (in this case Aged Care Crisis Centre above) collected and counted the failures that the "truthful deception" came out. The minister had to "fess up". The agency's own publication "The Standard" had it in a footnote which only a skilled lawyer looking for flaws would have looked at critically enough to pick up.
*Data is at 31 December 2006 and comprises 2,872 accreditation decisions from a home's last site audit or review audit. The same criteria were applied to data as at the end of 2003 and 2000 so that a 'like for like' comparison was possible
Can you see it? On the 31st December 2006 less than 10% of nursing homes had not yet "fixed" their failures and succeeded in persuading the agency that they were now compliant with the standards they had failed. Imagine the industry's rush to do that before that key date and so keep the figure low.
Perhaps we should do our own maths and see what we get.
On the previous 3 year cycle at 31st December 2003 the figure was 88% - or 12% not 100% compliant. If we are generous and accept that those figures represent the average then the average number of homes not 100% compliant at its last check on every single day during that 3 year period was probably about 10%. How long does it take for a nursing home to fix a problem and get the agency to endorse that - days, weeks, months?. Lets be generous again and say 3 months.
So lets assume the 10% changes over, on average, about once every 3 months. So there are 12 cycles of 3 months in the year. So lets be more honest than the agency and the minister and calculate that, at a wild guess only, there were about 120% of homes not 100% compliant at some stage over the 3 years. No doubt some failed on several occasions. If we were even more generous used 6 months as the time it took them to fix problems then it would be 60%. That it took so long would be a pretty poor effort too.
Except that the minister left out the small footnote in her press release the report is absolutely correct and would stand up in a court of law. But do we as a community think that this is honest? Do we think the agency is acting for us? Do we trust it to monitor standards and protect us from rogue providers? Make up your own minds.
Let me quote again from the senate review of the 1997 aged care act. They were prophetic when they expressed their concern that
`a significant focus of the Agency will be the needs of service providers' to the detriment of consumer interests.
How did the other reviews treat the agency?
In spite of the lack of information about standards of care the productivity commission, examining nursing home subsidies in March 1999, wanted funding linked to standards of care.
Even if there were measures of care in place this sort of incentivisation was as likely to lead to some getting more money than they needed while others struggling with difficulties would be denied the support they needed to improve.
Crude marketplace logic might work after a fashion in a real impersonal market where ongoing collateral damage (casualties) are accepted. The market is a ruthless process in which many, even with the best of intentions and hard work succumb through no fault of their own. How many small Australian traders went to the wall when Woolworth's and Cole's set up in their towns. We have greater choice and ease of shopping as a result but it was not without considerable cost to some citizens. When applied to a sector, where collateral damage, measured in lost lives, is not legitimate, it turns common sense upside down.
The 2004 Hogan review praised the accreditation system as rigorous and effective. He accepted these sort of results and the method of reporting them as an indication that market pressures and the drive for commercial efficiency were not compromising care.
He recommended accreditation results where almost everyone got full marks be converted to a star system, which would give gullible consumers the illusion that it measured what they expected it to, and that almost all were 5 star.
The accreditation system was criticised in reviews carried out by the Senate Community Affairs Legislation Committee in November 2000 after the Riverside scandal. The minority report asked that it be urgently reviewed. The comments in the Senate Community Affairs References Committee in June 2005 were scathing. Accreditation was called a farce. The view was expressed that it "does not assess actual care delivered -- - - - - its capacity to provide objective information around care outcomes is limited".
The industry was itself critical of the accreditation industry at the 2009 inquiry by the Senate Standing Committee on Finance and Public Administration. While the community are angry that we do not get information that tells us about the care provided, the industry want
a next-generation compliance process - - - - - where the staff engage with getting better at what they are doing and the system works in favour of that, not just whether you are good or bad.
I would agree provided that we get another much better mechanism whereby we can learn what is happening to our seniors without having to send in a spy, and whether a nursing home is good or bad.
This organization has been heavily criticised by the public, by the press, and by a number of reviews. It does not do what we as a community want and expect. Accreditation and oversight are not compatible.
If accreditation helps the industry to improve services then none of us have a problem with that and it is commendable. If it is a vehicle to promote the industry we would have reservations. Even the ACCC requires advertisements to truthfully present the facts.
But its time we took the things that accreditation does not do away from this agency. Its time to create an organization that we can trust to do the things that accreditation does not do. Its time to have someone inside our nursing homes every few days so that they can tell us when things are beginning to slip long before they go off the rails. Most important of all, this should be one of us.
We should not get this out of proportion and start blaming people or the agency. We are looking at a social process that has gone very wrong.
Accreditation in 1997 was a popular belief system thought to improve care and probably did so. It was being promoted as a way of improving care and of ensuring that those groups who provided care followed processes which ensured care would be good. Around for a time, it had become the latest health care fad. Like all such ideas it was carried to excess and applied inappropriately. We live in a market society and advocates were out there selling their wares - in this case the process of accreditation. Like all salesmen they exaggerated. Failures don't feature in marketing. Critics had nothing to market. It was just what our politicians were looking for at that time.
Once established people who identified with the process and had promoted it would have been put in charge. They would have been highly motivated to make things work and would have marketed and sold it offering rationalisations and justifications for every failure and then believing their own explanations.
They built their careers and their identity doing this. Those who could not identify with it would have moved elsewhere. There is nothing new or unique about this or unusual that the people who remained and were successful were poorly suited to cope with the conflicts. The infallibility of the belief could not be challenged. They dug in and defended, doing whatever it took. We saw it with fascism (a belief system that led to the holocaust). We saw it with apartheid. In both instances those who were unhappy lay low and those who were deeply disturbed emigrated. These web pages describe the same behaviour in health and aged care in the USA. Isn't this what has happened with accreditation? Are we Australians so different to the rest of humanity that it cannot happen here?
We need to remember that the politicians who set this up and the people who organised and ran it really believed very deeply in what they were doing. We all look down our noses at fascism, apartheid, communism, fundamentalists and cults scoffing at what they do. We don't see these as red flags to problems in our nature. We see them as aberrations and believe we could never be like this. We have not yet learned to look instead at what that tells us about how we all behave and how we all come to believe in things and become committed to processes that go off at a tangent. Until we do so we will never learn to avoid this.
The complaints system has been extensively criticised by community groups, by families, and by the press. It is increasingly apparent that it has not worked for residents. It was severely criticised in the June 2005 report titled "Quality and equity in aged care". Witnesses and submissions described fear among, and intimidation of, family and residents who spoke out. They told of retribution against nurses who blew the whistle.
In October 2009 a report by Professor Walton confirmed many of the complaints. It found that the complaint system was too legalistic and focused on natural justice rather than resolution of the complaint. The department was not independent and should not be handing this. It seems that they permitted all this and probably discounted the allegations as due to interpersonal conflicts by disgruntled nurses and family. Walton has said it all and I do not need to go further here. Its not too long and its easy to read.
Walton recommended that a totally independent body be set up to handle complaints. In my view she did not go far enough. Without a local facilitator able to mediate and investigate tensions and anger will continue and we will not have issues resolved. That independent body must function locally in each community.
Investigation after investigation since 1997 has demonstrated the drop off in nurse numbers across Australia, and particularly in aged care where deskilling and the use of agency nurses or foreign nurses who are unable to relate as well to the elderly have compounded the problems.
In hospitals doctors confront management and so maintain a focus on care. Because they have "leverage" and can take their patients elsewhere, management has to confront and respond to their criticisms. They cannot continue to delude themselves and are forced to face up to the real world. Nurses have no leverage in aged care and can become demoralised as the focus shifts from care to profit.
While parity in payment, better staffing levels, a better mix, and multiple other issues need attention, I do not believe that we will have a motivated and caring nursing force until we move the focus back to care and until links with the supporting community are restored.
It is also clear from the senate Community Affairs References Committee June 2005, press reports, reported instances of failures in care, and statements by the AMA that doctors are no longer in attendance and geriatricians are not encouraged. Other medical services are in short supply and dental care seems to be almost non-existent.
The reason these people are going into a nursing home is that. as in every other disease process, their systems are failing and for this they need medical care. While in the community they would with rare exceptions have attended their doctors, dentists and probably physiotherapists or podiatrists regularly. At a time when they enter a nursing home these needs are increasing and ever more pressing.
There are additional medical decisions relating to palliation and termination of treatment that can only be effectively made by a medical practitioner who knows the patient, and their family because they have been in regular attendance. Ideally that doctor should have some expertise in caring for the aged. This cannot be left to nurse aids.
The current situation is not socially tenable.
The review "A Healthier Future for all Australians" by the National Health and Hospitals Reform Commission on June 2009 mapped out the digital future for health care and aged care is part of that future.
Computers and digital records are now the norm in general practice and soon should be in hospitals and nursing homes too. This is the era of cheap hand held devices with graphic interfaces, touch screens and WIFI connections so there can be no excuse for delays in making records. Any future planning for nursing homes must include these advances.
As a species we have mastered the intricacies of speech and many of us can speak more than one language. We have mastered the intricacies of writing, spelling and can handle typing and cursive writing extracting meanings. To suggest that we would not find tapping on visible symbols and sliders with perhaps a cursive explanatory note attached much easier to learn is nonsense. Children as young as five are pressing buttons on most of their toys. Almost everyone under 50 has runaway fingers on their mobile phones. This would be second nature to them. It would require a fraction of the training we have needed to develop other skills. There should be no need for most people to type.
It will save vast amounts of time making records if we log what is done with a tap on the panel at the foot of the bed. Management, nursing regulators and the community would all know how long it takes to do things and whether they have been done. People would obviously forget to tap or make mistakes and have to go back later to make corrections. That is not vital unless there is a dispute about what was done and when. The savings in staff time, in administration, in oversight processes and ultimately in cost might be enormous. It should be possible to put an iPad-like device in each room for less than $600 and that will keep falling.
A system like this may not be too expensive to install, nor is it rocket science to log call lights and their responses - one of the most sensitive measures of adequate staffing, yet one that is difficult to monitor from a distance.
Lets think about what is possible and what the future can hold - then work out how we can get as near to that as possible. This is the digital age, the information age. Its time to grasp it and make it work for us.
The issue of bonds and or payments from those who can afford them has been a matter of debate and of inquiries. The safety of the bonds has received much debate.
Recommendations in 1997 and again by Hogan warned that residents could lose all their money if a nursing home operator went under. This has happened and an embarrassed government had to dig into tax payers contributions to pay them.
Legislation was introduced and reviewed by the senate in March 2006. Providers were required to make contributions into a fund to repay bonds when they were lost. I recall the providers objecting strongly and I am not sure that this fund was ever set up.
Whether people pay bonds or contributions is a philosophical issue. Also whether they be permitted to pay for more. The democratic process needs to work it out.
I personally have no problem with those, who can afford it, making a contribution to their care provided it does not result in hardship for anyone. I also think that we have a responsibility to provide a good standard of accommodation, care and life to those who have been less fortunate. They cannot however expect us to provide them with a 5 star hotel when most of us don't enjoy that.
If someone has the funds and wants to pay for additional 5 star luxury and someone wants to provide it then I think that is their business provided their vulnerability does not lead to their being exploited and misused. Others may disagree.
What I am very concerned about is the negotiation of bonds between residents and provider mediated by the assessor. In this situation some providers will cherry pick residents able to pay bigger bonds and or fees. This means that poorer residents with greater need will be discriminated against. Those who will suffer are the unfortunate citizens left behind and identified as needing help by the Senate Standing Committee on Community Affairs inquiry "A decent quality of life" in March 2008
This is a "normal business practice" but is highly unethical within the health and aged care context. When Mayne Health did this doctors took their patients to other hospitals and the company almost went under. There is no one to do that in nursing homes.
Hogan was aware that this would happen in 2004 but showed little concern about it. He recommended that bonds be negotiated between resident and provider. These sort of negotiations are part of efficient business practices.
Information given to the inquiry by the Senate Standing Committee on Finance and Public Administration that reported in April 2009 indicated that cherry picking was occurring.
The next step is to pay commissions (a better word is kickbacks) to assessors to get them to advise wealthy potential residents to come to their nursing homes. That is not illegal in Australia either and is a common practice in other sectors. I will be very surprised if it is not occurring.
The final step in this process is to pay a bounty to induce assessors or others to become bounty hunters and go into the community to market their homes to the wealthy and persuade them to enter their nursing homes even when this is not required. When would this cross the boundary and become illegal?
I have battled since 1999 and more recently to have something done to control the sort of person or company that is allowed to care for the vulnerable. There is nothing new or unusual in doing this. It has been in existence for many (perhaps hundreds of) years and probity requirements are still in hospital legislation for all states.
In essence a probity requirement means that the protection of vulnerable people takes precedence over the rights of others to do business or provide a service. The applicant must show that they do not pose a risk to the vulnerable and the burden of proof is on them.
The amendments to the Aged Care Act made in December 2008 did not adequately address many of these issues. The current situation in which a business can buy a nursing home and buy the approved provider status attached to the home is not socially tenable. However deviant their conduct they are not required to seek approval to operate that nursing home.
Private equity investment has grown across the world and they have not been slow to enter health and aged care in the USA, Australia and elsewhere.
Private equity groups bring in managers who are further from the coalface, have less direct experience of the sector, and who increase the pressures for profit.
You would expect their ownership to impact adversely on a sector where profit and care compete directly for the same dollar.
This issue was put to the review of private equity investment by the Senate Standing Committee on Economics in August 2007. They did not accept this but only weeks later the New York Times published an expose of the consequences for nursing homes in the USA. A government inquiry followed and this resulted in considerable tightening up of regulations relating to ownership.
While there have been rumblings in Australia it is only recently that the high rate of failures in care and/or of accreditation in Domain Principal Group has been documented by the combined pensioners and superannuants association of NSW. The ultimate majority owner is AMP Private Equity. The nursing homes are part of their "social infrastructure fund" where it is managed together with roads, retirement villages, car parks etc.
Transparency has been left to near last because it applies to all of the other concerns above. We want to know what is happening in aged care. Several of the reviews have referred to transparency, the need for it and urged more of it. Many others have complained about it.
We must accept that real transparency will never occur while the providers, the government or any other agency they control hold the information we need. We should continue to press for control of the information so that we can supply it to government and industry and use it to negotiate our concerns.
Several of the reviews have urged greater involvement of the community in the processes surrounding aged care. That has not happened.
We are not going to get that unless the families and the communities of residents organise, press for it, show their determination to be involved, and play an active part in participating and controlling.
Knowing what has happened and analysing it critically is important in helping us avoid the same mistakes. Knowing the current situation and its problems is important. We know where we are starting from and can recognise limitations, then plan how we can get from there to where we want to be.
Lets not get bogged down in the past and in recriminations. Lets decide what we want and where we want to be and then have the courage and the vision to project ourselves towards it - not in a rigid and fixed way but step by reflective step being prepared to change direction and try another route when one does not work.
Whether you agree or dissagree with the argunments made here, the productivity commission has asked for our input. Its time to make submissions and tell them what we want and what we expect - a short letter is better than nothing. Go to http://www.pc.gov.au/projects/inquiry/aged-care for details and to see submissions. The closing date is 30th July 2010.
Oh! and please without more backbiting and scare mongering. By all means tell them what you think is wrong but don't forget to tell them what you expect in the future.
Click Here to go back to the main report page
|